Annual report 2020
In 2020, which was a particularly challenging year on account of the pandemic, the 1,112 employees at Schulthess Klinik showed how we can achieve positive results with team spirit, commitment, flexibility and plenty of new ideas. Thanks to them, we have been able to consistently pursue our primary goal of relieving people of their pain and restoring their mobility and, in doing so, living up to the trust of our patients.
“In a crisis, good becomes even better.”
Andrea Rytz, Director, CEO
Schulthess Klinik is one of Europe’s leading orthopaedic hospitals. As a specialist orthopaedic clinic, we focused once again in 2020 on offering first-class treatment for the musculoskeletal system. Schulthess Klinik focuses on orthopaedic surgery, spine neurosurgery, neurology, rheumatology, manual medicine and sports medicine. We are also a certified Swiss Olympic Medical Centre. Our specialist departments offer patients treatment that is backed up by science and excellent expertise, extensive experience and state-of-the-art facilities. Our patients benefit from the interdisciplinary collaboration between our departments as well as from our Research department, whose results are incorporated into everyday clinical practice at our facility. Schulthess Klinik accepts patients with both general and supplementary health insurance.
Founded in 1883, the clinic has been financially supported by the Wilhelm Schulthess Foundation since 1935. It has always preserved its character as a non-profit organisation Its long-standing tradition of research is a testament to the clinic’s commitment to continually improving treatment. Not only this, but we have also conducted over 153,000 patient surveys since 2004. With 409 publications and training courses to our name in 2020 alone, we were able to pass on our knowledge to colleagues both in Switzerland and abroad.
The excellent performance of our staff, great degree of trust of our patients and referring physicians
With 9,215 surgical procedures, 7,671 inpatients and 114,152 outpatient consultations in the past year, our statistics in these areas almost match those of 2019 – which seems unbelievable given the difficulties posed by 2020. It was a year of lockdowns, a vast number of uncertainties when it came to planning and, above all, a sense of unease that affected everyone. It was a year in which past decisions were often no longer valid in the present. But it was also a year in which our excellent corporate culture was strengthened even more by the crisis and the increased sense of togetherness was clearly noticeable.
Many people and entire professional groups, who would usually do most of their work behind the scenes, suddenly moved into the foreground. This means we have all become much more aware of how important many areas of work are that we otherwise often take for granted. The impeccably hygienic cleaning of our work areas and equipment, the IT support for remote working, the technical service on site and the logistics, which needed to be quickly adapted to constantly changing situations, are just a few of the many examples.
Team spirit, commitment, flexibility and plenty of new ideas achieved lots of positive results. This contributed to the fact that we were able to live up to the long-standing great degree of trust that our patients and referring physicians have in us, even during the crisis.
We would like to thank our patients and referring physicians for having had an enormous amount of trust in us. We would also like to thank our 1,112 colleagues at the clinic, of whom we are very proud, for their extraordinary commitment in 2020.
Shoulder and Elbow Surgery

Our range of services in shoulder and elbow surgery is comprehensive. Whether it be fractures, ligament or tendon injuries or diseases caused by wear, such as osteoarthritis – our specialists cover the entire spectrum of treatments with both conservative and surgical approaches, including complex revision surgery. This involves doctors working closely with our Research department, which means scientific research can be incorporated directly into everyday clinical practice and, in turn, practical experience can influence research results.
“The digitalisation of scientific conferences has meant that we have been able to reach many more people than with in-person-only events, which allows us to share our knowledge.”
Prof. Dr. med. Markus Scheibel, Head of Shoulder and Elbow Surgery
The Shoulder and Elbow Surgery department at Schulthess Klinik is looking back on a challenging but exciting year. We had to break new ground, especially in the areas of professional exchange and teaching. Thanks to the great commitment of our staff, we kept caring for our patients via video and telephone consultations, even during the lockdown . In fact, we are pleased to report that we were even able to increase the number of interventions compared to the previous year. This represents a display of trust on the part of our patients and referring doctors that we greatly appreciate.
Leading and participating in conferences all around the world
Sharing our knowledge with colleagues in Switzerland and abroad is an important part of our work. In September, for example, we teamed up with our other partners to organise the Society for Arthroscopy and Joint Surgery (AGA) Congress. Our specialists also spoke at the Annual Congress of the German Society of Shoulder and Elbow Surgery e.V. (DVSE). The two conferences, originally planned to take place in Davos and Düsseldorf respectively, were held online for the first time in the history of the two societies due to the pandemic – and both turned out to be a great success. This wide online reach allowed us to gain a much larger audience than we ordinarily would with in-person-only events, enabling us to offer extremely efficient training.
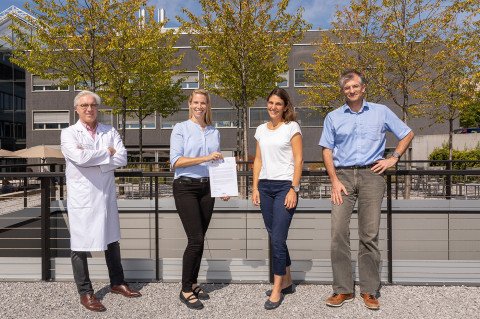
Contract for the 2023 DVSE Annual Congress
Schulthess Klinik and Balgrist University Hospital have been awarded the contract to hold the 2023 DVSE Annual Congress. We are delighted to be able to bring this leading scientific congress in shoulder and elbow surgery to Zurich for the first time.
New surgical technique to treat glenoid defects in patients with shoulder instability
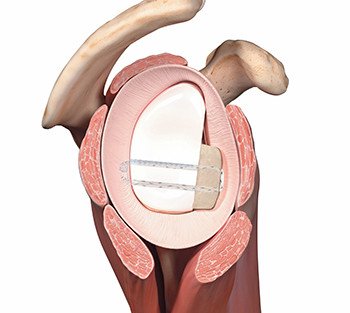
We introduced arthroscopic glenoplasty with bone chip grafts, a major advancement in existing surgical techniques, for the treatment of defects of the glenoid (socket) in patients with shoulder instability. Unlike the bioabsorbable screws or metal implants used previously, this technique involves fixing the chip using FiberTape® Cerclage. With this technique, complications from the aforementioned implants can be avoided and the subscapularis muscle (important for internal rotation of the shoulder) is spared.
Academic projects and publications
Together with our Research department, we launched a series of promising and future-oriented projects. For example, we established the world’s first detailed clinical register on injuries of the acromioclavicular joint. We have also made important progress with the “Surgical safety and effectiveness in orthopedics: Swiss-wide multicentre evaluation and prediction of core outcomes in arthroscopic rotator cuff reconstruction” research project, which is supported by the Swiss National Science Foundation (SNSF). The project takes a multicentre approach to predicting outcomes after arthroscopic rotator cuff reconstruction.
We also finalised several publications on topics such as “Sports ability and shoulder endoprosthesis”, “Early detection of implant loosening in anatomical shoulder endoprosthesis” and “Optimisation of clinical outcome after inverse endoprosthesis”.
Further information
Hand Surgery

Our Hand Surgery department treats injuries and diseases that affect the hand, forearm and peripheral nerves. We offer a comprehensive range of surgical and non-surgical treatments and draw on our many years of experience and scientific research to always look for the best solution for the patient.
“Despite the six-week lockdown in the spring, we came very close to maintaining the same number of consultations and interventions as in the previous year. This is proof of the great degree of trust our referring colleagues and our patients have in Schulthess Klinik, a fact with which we are truly overjoyed.”
Dr. med. Daniel Herren MHA, Head of Hand Surgery
2019 JHSE Editors’ Award for study on trapeziometacarpal osteoarthritis
The “Journal of Hand Surgery – European Volume”, the most renowned international specialist journal in the field of hand surgery, gave the 2019 JHSE Editors’ Award to one of our studies. The study addresses the question – at what level of pain and limitation of hand function is it best to operate on patients with osteoarthritis of the thumb carpometacarpal (CMC) joint in order to achieve the best possible outcome? The results will help doctors to advise patients on the most appropriate time to have surgery.
The “Journal of Hand Surgery –European Volume” does not end up featuring even 20% of the articles submitted for publication as they are subject to a rigorous peer-review process conducted by several independent experts to ensure academic quality. The JHSE Editor’s Award is presented to the six best articles published in the journal in the previous year.
Dr. med. Daniel Herren takes office as FESSH Secretary General.
In September, our Head of Hand Surgery, Dr. med. Daniel Herren MHA, took office as Secretary General of FESSH. FESSH is the European umbrella organisation of national societies for hand surgery and its main aim is to promote cooperation between hand surgeons in Europe.
The Secretary General is the chairperson of FESSH and its various committees. After six years on the Board of Directors as Finance Officer, Daniel Herren was elected for a three-year term of office. During this time, he mainly plans to further promote the training of young hand surgeons, research and communication between European hand surgeons.
Innovation and continuity in joint replacement

An important part of our treatment in hand surgery is the use of artificial joints. The choice of the appropriate prosthesis and our specialists’ extensive experience with the associated surgical techniques are important factors here. We are also actively involved in the development of prostheses – the CapFlex finger joint prosthesis, for example, was developed at Schulthess Klinik. By the end of 2020, we used 333 of these in total at our clinic, and the prosthesis has already been used over 1,000 times outside of Switzerland. We have also amasses a great deal of experience with thumb carpometacarpal (CMC) joint prostheses. For example, we already implanted 135 of these in 2019 and 2020, which is the most to be used in Switzerland.
Further information
Hip Surgery

Today, the Hip Surgery department at Schulthess Klinik is Switzerland’s largest centre of excellence in this area. Every year, the highly specialised team led by three renowned professors gives patients almost 1,200 hip prostheses, including during complex revision procedures. In addition, they also perform complex joint-preserving surgical procedures, including hip arthroscopy, osteotomies in children and adults, and cartilage repair procedures. All procedures are monitored by our research team with regard to short-term and long-term results, a process which enables continuous improvement in the quality of treatment.
“We were impressed that most patients were understanding of the restrictions imposed by the pandemic, despite the considerable suffering they were enduring. A great number of operations and consultations had to be postponed at the time.”
Prof. Dr. med. Michael Leunig
Revision rate: Twice better than the Swiss average
The Swiss National Joint Registry, Hip and Knee (SIRIS) is a database for orthopaedic specialists, hospitals and the implant industry, and it serves as a quality assurance instrument. Recording all hip and knee prosthesis operations in one central place, i.e. in the SIRIS, has been mandatory since 2012.
Concrete conclusions can be drawn from the data recorded in past years, especially with regard to revisions (prosthesis replacements). For example, the two-year respectively five-year revision rate for first-time hip prostheses is measured, i.e. how many patients require another surgical procedure on the artificial joint within two years respectively five years of the initial operation. For several years now, the revision rates for our patients have been significantly lower than the Swiss average, both after two and after five years. In the study period from 2012 to 2020, this amounts to 1.1% respectively 1.4% at Schulthess Klinik, which is less than half the Swiss average (2.6% respectively 3.5%). The fact that specialised centres with very large numbers of cases have a lower revision rate is observed in practically all health care systems internationally.
Since 2015, Schulthess Klinik has been digitally recording data and transmitting it to the SIRIS register immediately after the operation, and this is done by the surgeon personally, which results in high data quality.
Decades ago, with its arthroplasty consultation, Schulthess Klinik started recording and following more than the purely technical side of prosthesis surgical procedures. In order to measure individual patient satisfaction, about 15 years ago, we also began to systematically question our patients about their subjective health using standardised questionnaires. This means the combination of these two sets of data gives us a comprehensive overall picture that allows direct conclusions to be drawn about our treatment methods and their quality – all in all, aspects that are now also being included in the expansion of the SIRIS database throughout Switzerland.
We will continue rigorously pursuing this path in the coming years with the aim of continuously improving quality.
Cartilage surgery of the hip – standards and new developments
Cartilage damage to the hip can occur even at a young age, especially if deformities such as impingement are present. If these kinds of deformities, some of which are subtle, go untreated, they can lead to a mechanical conflict between joint structures, thus causing premature wear of the joint and osteoarthritis at a young age. Treatment is most successful when given before the onset of cartilage damage and involves correction of the deformity. If cartilage damage is already present, it may need to be treated in order to prevent the joint damage from spreading.
Microfracture (MFx) is a technique that has been in use for a long time and is particularly suitable for minor defects. Cells from the bone marrow flow into the defect from tiny holes drilled into the bone of the damaged area, which helps to form replacement cartilage. Modern cartilage repairs such as the AMIC technique or One-Step Autologous Minced Cartilage Procedure are technically more demanding and require greater experience. These techniques are also used regularly at Schulthess Klinik.
AMIC technique in cartilage damage
A further development of microfracture (MFx) is the AMIC technique, in which the cartilage damage treated with MFx is covered with a stabilising collagen membrane. This provides local protection for the bone marrow cells repairing the defect, and the quality of the developing replacement cartilage is more stable, which improves clinical outcomes. Sewing in the AMIC membrane is technically demanding and must therefore be carried out via an open surgical procedure.
One-Step Autologous Minced Cartilage Procedure
Another facet of cartilage repair is the technique referred to as the One-Step Autologous Minced Cartilage Procedure. Cartilage tissue is removed from the edge of the defect area to be treated and ground into the tiniest possible pieces of “minced cartilage”. These are then returned to the area of cartilage damage where the chips mature into very stable and much more resilient cartilage. This technique is still new, but its use in the knee joint has already been researched in initial scientific studies. The findings tend to show better results than the other two methods mentioned. At Schulthess Klinik, we have already successfully applied this promising procedure to the hip several times.
Further information
Knee Surgery

The Knee Surgery department at Schulthess Klinik is Switzerland’s largest reference centre for knee joint replacement. The department performs around 850 knee replacement procedures each year and also carries out complex revision operations. In addition to prosthetics, our specialists offer the entire treatment spectrum for diseases and injuries of the knee. This ranges from non-surgical treatment techniques to cartilage repairs and axial corrections to the treatment of fractures and complex ligament reconstructions.
“Lots of things just had to be implemented in times of need. In this way, the pandemic acted as a positive accelerator and showed, in many cases, what can be achieved within a short period of time and without extensive prior planning.”
Dr. med. Thomas Guggi, Senior Consultant for Knee and Hip Surgery
The two-year revision rate for total knee replacements is half the Swiss national average
The Swiss National Joint Registry, Hip and Knee (SIRIS) is a tool that can be used to assess the quality of orthopaedic specialists, hospitals and implant industry companies. Since 2012, recording all hip and knee prosthesis operations in one central place, i.e. in the SIRIS, has been mandatory. Currently, every 24th knee prosthesis surgical procedure recorded in the register was performed at Schulthess Klinik.
Concrete conclusions can be drawn from the data recorded in past years, especially with regard to revisions. The two-year respectively five-year revision rate for first-time knee replacements – i.e. the percentage of patients who require a revision operation within two years respectively five years after the original replacement – is measured this way. For several years now, the revision rates for our patients have been constantly significantly lower than the Swiss average, both after two and after five years. In the study period from 2012 to 2020, this amounts to 1.4% resepectively 2.9% at Schulthess Klinik, which is less than half the Swiss average (3.3% respectively 5.4%). With regard to the ten-year figures, the comparison is likely to be similar.
Since 2015, Schulthess Klinik has been digitally recording data and transmitting it to the SIRIS register immediately after the operation, and this is done by the surgeon personally, which results in high data quality.
Early on, Schulthess Klinik started recording and tracking more than the purely technical side of prosthesis surgical procedures. For years, patient-specific assessments have also been systematically collected based on standardised questionnaires (patient-related outcome measures – PROMs). This means the combination of these two sets of data gives us a comprehensive overall picture that allows direct conclusions to be drawn about the quality of treatment – all in all, aspects that are now also being included in the expansion of the SIRIS database throughout Switzerland.
We will continue rigorously pursuing this path in the coming years with the aim of continuously improving quality.
Very low rate of infection for knee replacements compared to the Swiss national average
The Swiss Registry for Surgical Site Infections managed by Swissnoso is another important tool for assessing the quality of hospitals. The majority of Swiss hospitals have been participating in the registry system since 2009. One out of every 12 knee replacements registered in the period between 1 October 2018 and 30 September 2019 alone was performed at Schulthess Klinik.
The rate of infection one year after a knee replacement is the most important quality criterion here which, in the evaluation period, was 0.28% at Schulthess Klinik (Swiss average: 0.76%). Thus, the risk of an infection during the insertion of a knee prosthesis at Schulthess Klinik is only slightly more than one third as high as the Swiss average.
Patella prosthesis: When osteoarthritis first affects the patella
If all non-surgical treatment methods for knee osteoarthritis have been exhausted and joint-preserving surgery is not (or no longer) an option, a joint replacement may be considered. It then has to be decided whether the entire knee joint should be replaced with a total prosthesis, or only the diseased part with a partial prosthesis.
If the osteoarthritis only affects the patella, what is known as a patellofemoral prosthesis can be considered. Other requirements for this are a straight leg axis and stable ligaments. The advantage of this method is that it really only replaces the diseased knee compartment. The rest of the joint, menisci and cruciate ligaments are not affected. Expected benefits for the patient are a more natural-feeling knee, free mobility and an overall tendency towards better function than with a total knee prosthesis. The excellent results are confirmed both among our patients and in current scientific studies.
Thus, in our clinic, we check precisely which compartments are affected in every case of osteoarthritis. If it is purely a matter of patellofemoral joint osteoarthritis, we decide on a case-by-case basis whether patellofemoral arthroplasty is possible.
In 2020, we inserted 751 total knee prostheses and 115 partial knee prostheses at Schulthess Klinik. Of the partial knee replacements, 12 were patellofemoral replacements.
Autologous minced cartilage repair: gentle and economical
Cartilage defects in the knee joint are becoming increasingly common, especially in younger patients, and are very often due to accidents. The aims of treatment are to relieve pain and improve physical activity, but also to prevent secondary damage such as early-onset osteoarthritis. Several surgical methods are available for the treatment of these kinds of defects. A current technique involves using “minced cartilage”, also called autologous cartilage repair. Cartilage is removed directly from the margins of the area of cartilage damage, carefully cut into tiny pieces (minced) and then mixed directly with the patient’s own blood. The blood is taken during the surgery and processed into platelet-rich plasma (PRP) with a centrifuge. When combined with the minced cartilage, the PRP serves as a vehicle for it, acting directly as a “tissue adhesive” after implantation. This holds the transplanted cartilage in place in the defect. New cartilage forms over time as the cartilage cells grow out of the minced pieces. This process is stimulated by the PRP, which regulates excessive inflammation of the entire joint at the same time.
In the past, Autologous Cartilage Transplantation (ACT) was the method used in most cases. However, ACT requires two operations to complete the transplantation process. First, cartilage must be removed in an initial operation and then cultivated in the laboratory. The cartilage cells can only be used again after cultivation, four to six weeks after the first operation, in a second open surgical procedure. With autologous cartilage repair, on the other hand, this is all done in a single operation, and usually arthroscopically, i.e. with the smallest of incisions. This is gentler for the patient and ultimately more economical. Rehabilitation is faster. At Schulthess Klinik, we have been using this procedure for a number of years because of our good experience with it and we have recently been using the arthroscopic technique more and more. The positive results are proven, among other things, in the clinic’s own studies on cells and clinical studies.
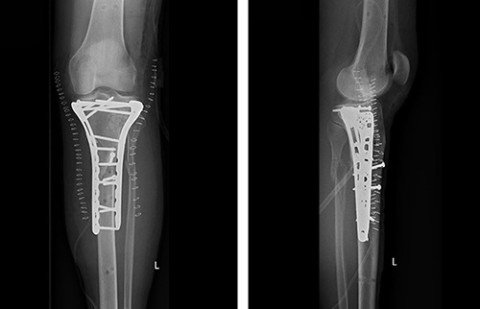
Fracture treatment
Increasingly, we are also taking on complex fracture treatment such as tibial plateau fractures. These kinds of fractures often occur in winter sports accidents. After initial assessment and primary care on site, patients often want to be treated close to home. To facilitate this, a transfer can be organised via our Ortho-accident helpline.
In the case of fractures affecting the joint, it is important to restore the form and function of the joint to avoid premature signs of wear and tear. This is ensured with special plates and bone augmentation. These X-rays are from a patient who was injured in a skiing accident. After the diagnosis was made and external stabilisation was fitted, the patient was transferred to our clinic. Once the swelling in the soft tissues had gone down, we performed a repair using plate osteosynthesis.

Further information
Foot Surgery

Our Foot Surgery department treats diseases and injuries of the foot and ankle. The medical team consists not only of surgeons, but also doctors who treat patients in a purely conservative way, i.e. non-surgically. This also involves a close interdisciplinary exchange within the hospital, with the Sports Medicine and Physiotherapy departments, for example.
“By maintaining close communication with our patients, we were able to help them with treatment again immediately after the lockdown.”
Dr. med. Thomas Rutishauser, Senior Consultant in Foot Surgery
Like all other specialist departments at the clinic, foot surgery was also affected by the complete lockdown in place in the spring. We had to postpone all operations planned for this period. We did, however, manage to stay in close contact with our patients and make fresh plans to the extent possible. This meant that we were able to resume surgical operations from the first day after the lockdown and were immediately working at full capacity. Within a short time and in compliance with the pandemic guidelines, we were also able to have consultations with patients again. The fact that our patients wanted to return to the clinic soon after the lockdown at such an uncertain time shows how much they trust in us – something we greatly appreciate. We would also like to thank our referring doctors for their excellent cooperation and trust throughout the year.
Workshops for referring doctors
The interdisciplinary workshop for our referring doctors, held by teams from the Foot Surgery and Rheumatology departments, got off to a promising start. That being said, however, we were unable to continue with the training sessions, which unfortunately fell victim to the pandemic. But the keen interest shown by the GPs is reason enough to resume training as soon as this is possible again.
Further information
Spine Surgery, Orthopaedics and Neurosurgery

The specialist Spine Surgery, Orthopaedics and Neurosurgery team treats injuries and diseases of the spine. Degenerative diseases, deformities and inflammation belong to the spectrum of conditions the team treats in addition to fractures and tumours. Depending on the condition in question and its severity, the treatments range from various conservative (non-surgical) techniques to extremely complex surgical interventions including revision surgery.
“Our team remained motivated, flexible and fully committed to our patients, despite the constantly changing conditions dictated by the pandemic.”
Tatjana Krieger, Practice Manager of Spine Surgery, Orthopaedics and Neurosurgery
The Spine Unit is 33 years old
Treating back pain can involve many different medical disciplines that need to work together to achieve the best possible outcome for the patient. The Spine team at Schulthess Klinik recognised this a long time ago, which led them to found the Spine Unit in 1987, which was the first interdisciplinary team unit of its kind at the time in Europe specialising in spinal conditions. Multidisciplinary care for patients with spinal column conditions has always been its focus.
Surgeons work very closely with neurologists on everything from assessment and treatment to intraoperative neurological monitoring during challenging spine surgery. Surgical and conservative specialists work hand in hand. Our spine surgeons are in close contact with our other conservative departments, i.e. those that treat patients without surgery, including Rheumatology, Manual Medicine and Physiotherapy. Likewise, it goes without saying that the scientific focus and commitment to research and teaching are a central element of the work in this area.
Interdisciplinary training in spinal health for GPs
GPs also play an important role in the treatment chain for the widespread disease of back pain, which is why our interdisciplinary Spine team invited GPs to attend a training session in February. They received a scientific overview from the specialist areas of neurology, rheumatology, radiology and spine surgery, orthopaedics and neurosurgery, each with a discussion of how this information can be useful in their everyday practice. In keeping with the anniversary of the Spine Unit, the topic of back pain was not only examined from a surgical perspective, but as a holistic, interdisciplinary topic.
Scoliosis surgery
Our spine surgery team treats scoliosis patients in multidisciplinary cooperation with our Paediatric Orthopaedics department. Most of our patients (over 90%) are treated conservatively, i.e. without surgery. In those cases where surgery is necessary, we can offer the whole spectrum of surgical treatment methods, including posterior open or minimally invasive correction procedures, anterior corrective surgery with reinforcement or anterior or posterior growth guiding measures (with tethering procedures that preserve mobility, see below), as well as complex surgery for severe scoliosis or revision surgery. Having such a vast array of approaches means we always employ the surgical method that is most suitable for the patient in question. Although we opt for predominantly conservative scoliosis treatment, our surgical case numbers are still very high, with over 47 major scoliosis operations performed in 2020. Our surgeons therefore have many years of extensive experience.
New scoliosis surgery methods designed to preserve mobility successfully introduced
In March, two scoliosis operations were performed at Schulthess Klinik based on a new procedure – one that had never been used before in Switzerland – that is designed to preserve mobility. The method is a flexible correction of the curvature which is then guided by further growth. The first two operations were performed by visiting professor Peter O. Newton, M.D., from San Diego assisted by Prof. Dr. med. Dezsö J. Jeszenszky and Dr. med. Tamás Fekete from our spine surgery team. Since then, this surgical method has been used on a regular basis at Schulthess Klinik.
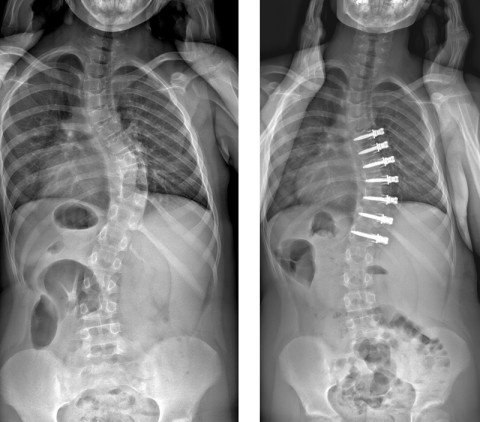
Although this surgical method is only suitable for a few patients, namely children, who are still growing, it offers them a number of significant benefits. This is because, in contrast to the formerly used standard technique, no spinal fusion is performed on the affected vertebrae. The spine remains mobile, the intervertebral discs are less affected and, in the best case, only one operation is necessary. The minimally invasive approach also results in less blood loss and usually less pain.
Complex revision surgery
In 2020, Schulthess Klinik was again requested to take on various complex revision cases following multiple scoliosis operations. In particular, there were patients from Germany and Austria who could not be accepted by any hospitals in their home countries. We accepted these patients and were able to help them. This was possible thanks to a perfect combination of essential factors: many years of experience, intraoperative 3D imaging and intraoperative, multimodal neuromonitoring supervised by a dedicated Neurology team made up of highly trained senior physicians.
Long-term results in research into lumbar stenosis
Lumbar stenosis is a common spinal condition in which the spinal canal narrows in the lumbar region and can lead to pain, sensory disturbances or even paralysis. There are numerous options for treatment with and without surgery. Unfortunately, nerves damaged by lumbar stenosis have a very small chance of recovery. This makes it all the more important to treat patients suffering from this disease at the right time and with the right method for their particular case.
In 2011, a multicentre observational study was launched under the coordination of the Horten Centre of the University of Zurich in order to enable this treatment, which can be optimised for individual patients, to be developed. More than 850 patients from Schulthess Klinik, Balgrist University Hospital, University Hospital Zurich and other Swiss hospitals were observed for three years. More than one third of the patients in the study, and thus clearly the largest proportion, came from Schulthess Klinik. The results have led to 24 studies so far, with the aim of providing patients affected with optimal, knowledge-based and individual treatment. In particular, the long-term results comparing patients with surgical and non-surgical treatment were published in 2020. An excerpt of the comprehensive results of the study was presented to an audience of professionals from the field at University Hospital Zurich in January. PD Dr. med. François Porchet, the person mainly responsible for Schulthess Klinik’s part of the study, had the pleasure of welcoming Prof. em. Jeremy Fairbank, Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences at the University of Oxford.

Preparation for the Swiss National Joint Registry, Hip and Knee (SIRIS)
From January 2021, the Swiss National Joint Registry, Hip and Knee (SIRIS) will also be used throughout Switzerland for the spine (SIRIS Spine). SIRIS is a quality assurance instrument for orthopaedic surgeons, hospitals and the implant industry with a view to improving the quality of care. Since 2004, Schulthess Klinik has been routinely documenting all operations in a format that is compatible with SIRIS (Spine Tango). This and our preliminary work overseen by Dr. med. Frank Kleinstück, Co-Head of Spine Surgery, Orthopaedics and Neurosurgery and member of the SIRIS Scientific Advisory Board Switzerland, on the implementation of an electronic documentation system were then the ideal preparation. We were thus able to meet the requirements of SIRIS without any problems and are ready to begin entering data in 2021.
Professorship for Dezsö J. Jeszenszky

On 8 September 2020, the University of Debrecen in Hungary awarded Dezsö J. Jeszenszky the title of professor during a formal ceremony. His postdoctoral thesis describes “New surgical procedures in the treatment of paediatric spinal column diseases” and addresses questions that have accompanied him all his life as a spinal surgeon, namely how to keep improving treatment for patients. His thesis summarises what Prof. Dr. med. Dezsö J. Jeszenszky, with his pioneering spirit, has achieved over all the years of his career for the treatment of children with scoliosis and other spinal disorders.
Further information
Paediatric Orthopaedics

Providing personal and child-friendly care has always been the credo of the Paediatric Orthopaedics department at Schulthess Klinik. The more than 10,000 outpatient consultations we held compared to the 586 children and adolescents who underwent surgery demonstrate perfectly that our treatment in this area is predominantly conservative. Close contact with parents and referring doctors is as much of a given to us as interdisciplinary cooperation with the other specialist departments at the clinic.
“Not even the masks could get in the way of the trust we have with our young patients.”
Dr. med. univ. Hannes Manner, Co-Head of Paediatric Orthopaedics

What is really hard to believe is that, only in January, we held our annual paediatric orthopaedic examination course, which is very popular with paediatricians, in the large auditorium without any protective measures against coronavirus. Looking at these pictures seems almost surreal from today’s perspective. Less than two months later, we found ourselves in a time of great uncertainty – and yet we can now reflect on the most successful year ever for paediatric orthopaedics at Schulthess Klinik.
Running smoothly again after the lockdown
Despite the six-week surgery and consultation ban during the coronavirus lockdown, the number of outpatient consultations with children in our department increased to over 10,000 last year. The excellent infrastructure of the clinic, the effective organisation and the initiative of our colleagues made it possible for us to resume our paediatric orthopaedic care without a hitch at the end of April. At the same time, compared to previous years, there was a noticeable flexibility of patients and their parents towards appointments due to the ongoing school closures. We would also like to thank our many referring doctors for their continued trust in our work.
A trusting relationship as the be-all and end-all
We had great respect for how the children and young people would react to us masked doctors in consultations. However, we soon realised that this was not really a problem. On the one hand, their parents undoubtedly prepared them for this situation and, on the other hand, it is likely the eye contact and the empathy we practise that foster the trust that is so important for an optimal patient-doctor relationship.
Routine operations as well as complicated reconstructive procedures
We can also report an increase of 10% in surgical treatment. All in all, we operated on 586 children under the age of 16 in the Paediatric Orthopaedics department. In addition to routine operations, we also performed many complicated reconstructive procedures.
For example, we treated a 9-year-old girl who suffers from a very rare, serious disease involving the growth plates on one side of her body (Ollier’s disease). In autumn 2020, we were able to implant a Precice magnetically driven intramedullary lengthening nail (NuVasive®) during the correction of a 30-degree varus malposition of the thigh using an External Remote Controller-driven fixator, which enabled us to gradually lengthen the leg by five centimetres.
Another highly complex problem was presented by an infant, who had already been treated outside the hospital, with a persistent bilateral hip dislocation that could not be reduced conservatively, although we had tried all non-surgical options. We therefore performed a bilateral open hip reduction in one session. The success of this operation is due both to the considerable experience of the surgeons involved and the excellent work of our paediatric anaesthetists. The family-friendly rooming-in option at Schulthess Klinik and the wonderful nursing staff on our paediatric ward had an enormous impact on the speedy recovery of the infant.
Further information
Neurology

With a broad-based team of experts consisting of ten experienced neurologists, the Neurology department offers diagnostics and treatments spanning the entire neurology spectrum. Due to the close interdisciplinary cooperation with our orthopaedic departments, our focus is on peripheral neurology, i.e. nerve disorders of the spine, arms and legs. It is with dedication and competence that we also care for patients from all other areas of neurology including dizziness, Parkinson’s disease, multiple sclerosis, dementia, epilepsy and headaches. We also have various special consultations, for example regarding nerve ultrasounds, dizziness, Parkinson’s disease, fatigue or botulinum toxin for dystonia.
“Despite the difficult circumstances brought about by the coronavirus pandemic, we have been able to ensure continuity and safety in the care and treatment of our patients.”
Dr. med. univ. Christian Lanz, Head of Neurology
The coronavirus pandemic brought about significant, challenging circumstances for the organisation of our neurological department (located in a large orthopaedic clinic). We are proud to have managed to take very good care of our patients under these circumstances and to maintain continuity in treatment.
Further training under unique circumstances
For years now, Schulthess Klinik neurologists, under the direction of Dr. med. Ute Kretzschmar, have been regularly invited by the medical training organisation “Forum für medizinische Fortbildung” to speak on various subjects in the world of neurology. It is a well-known further education platform for internal medical specialists and general practitioners. This year, the lectures were held online.
The Spine Unit is 33 years old
The Spine Unit at Schulthess Klinik is an interdisciplinary team unit dealing with all aspects of the spine. The unit celebrated its 33rd birthday in 2020. Multidisciplinary care for spinal column patients is the focus here. The Neurology department plays a central role in this, providing support in diagnostics, treatment or in the electrophysiological monitoring of demanding spinal surgeries. Multimodal intraoperative monitoring is key when it comes to keeping a close eye on spinal cord and nerve root functions. This expertise has been built up and continuously improved over the last 20 years, under the watchful eye of Dr. med. Martin A. Sutter.
Acting as CYBATHLON medical partner
People with physical disabilities compete to master everyday tasks. In order to reduce physical limitations, internationally high-ranking technical universities around the world have developed a series of innovative, state-of-the-art technical assistance systems. For people who use these assistance systems, ETH Zurich has organised an international competition – CYBATHLON 2020.
Schulthess Klinik is supporting the event as a medical partner. The Neurology department, headed by Dr. med. Zina-Mary Manjaly and Prof. Dr. med. Jiri Dvorak (Consultant to the Board) organised the neurological examinations and checked the required inclusion criteria of all participating teams around the globe (from Japan to South Africa). Due to the coronavirus pandemic, most of the examinations were organised virtually with treating doctors on site. The competitions also took place virtually this year, unlike CYBATHLON 2016, which was held in Kloten.
Further information
Anaesthesiology

The anaesthesia team accompanies patients before, during and after an operation; the choice of the appropriate anaesthesia is only one aspect of this. Even in difficult times like during the pandemic, patient safety is paramount.
“Our Anaesthesiology team showed absolute commitment and flexibility and supported the neighbouring intensive care unit of the Klinik Hirslanden.”
Prof. Dr. med. Christoph Hofer, DESA, Head of Anaesthesiology
Always there for patients, even in difficult times
Even in difficult times, ensuring that our patients receive safe care is the top priority for the experienced Anaesthesiology team. This begins with deciding whether general anaesthesia, local anaesthesia or a combination of the two is the most suitable and safest approach for the individual operation. Having a comprehensive picture of the patient’s health is crucial for this. If necessary, this requires routine examinations by a GP and further clarifications by specialists.
Good preparation is essential, especially during the Covid pandemic, because certain operations have to be postponed due to the patient’s state of health. For other patients, their health condition must first be improved to prevent them suffering any problems with their health after the operation.
Specialised expertise and experience
During the operation, the Anaesthesiology team continuously monitors patients for depth of anaesthesia, cardiovascular function and respiration. This continues after the operation and the anaesthesia itself. Depending on the situation, care is given for different lengths of time in the Intermediate Care Unit (IMC), a specialised monitoring ward.
Owing to training and experience, the Anaesthesiology team was also able to support the neighbouring intensive care unit of the Klinik Hirslanden over the past twelve months during the Covid pandemic by providing medical equipment and staff.
Rheumatology and Rehabilitation

Rheumatology is a broad medical specialty. The conditions treated within this area of medicine range from a wide variety of inflammatory diseases, such as arthritis, to osteoporosis and degenerative spine and joint diseases. Thus, the Department of Rheumatology and Rehabilitation is a central interface for interdisciplinary diagnosis and treatment.
“In the pandemic year, we have once again come to value the personal consultation at the clinic.”
Dr. med. Adrian Forster, Head of Rheumatology and Rehabilitation
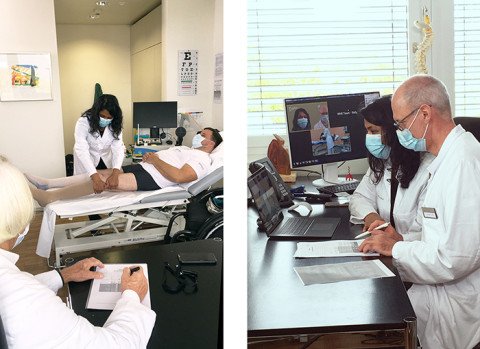
In 2020, the year of the pandemic, our experience of the possibilities and limits of telemedical care was intense. Of course, we also tried to continue to care for our patients as comprehensively as possible during the lockdown in spring. Telemedicine offered a good substitute for this to patients we already knew. This meant we were usually able to get a good grasp of their situation over the phone and offer them supportive advice. With new patients, on the other hand, both we and the patients were grateful that we were able to welcome them in person at the clinic again after the lockdown. Nothing can replace a face-to-face consultation. Especially in Rheumatology, where we look at patients in as holistic a way as possible, a comprehensive overall impression based on a physical examination combined with an individual conversation with the patient is crucial.
Osteoporosis consultations
The osteoporosis clinic offered by the Department of Rheumatology and Rehabilitation is increasingly being used, and is how we carried out 634 osteological assessments in 2020. These each include a bone density measurement (osteodensitometry with DXA), which is carried out on three parts of the body, namely the lumbar spine, hip and forearm. In addition, the Trabecular Bone Score (TBS) is calculated, which allows us to draw conclusions about the bone microstructure. If necessary, we also perform morphometry of the thoracic and lumbar spine (lateral fracture screening).
During the consultation, we record the risk factors and assess the fracture risk. Based on this, we develop treatment options that are tailored to the individual needs of the patient. In cases of severe osteoporosis, we use a number of specific medications in succession, or even simultaneously, to restore good bone stability as quickly as possible. In addition to teriparatide, we have recently been able to offer another treatment that stimulates bone formation, namely with the sclerostin inhibitor romosozumab. In the meantime, it is almost always possible to establish an effective and tolerable therapy.
Further information
Manual Medicine

Manual medicine has a tradition at Schulthess Klinik that spans several decades. With specific forms of manipulation, trigger point treatments and pain interventions such as infiltrations under X-ray or ultrasound, our specialists help with back problems as well as diseases of the peripheral joints such as the shoulder, elbow, hand, hip, knee and foot.
“Despite the pandemic, the increased demand for our treatments has continued from 2019. We are delighted that our patients and referring colleagues have placed such trust in us.”
Dr. med. Gérard Hämmerle, Head of Manual Medicine
Expansion of staff numbers
In 2019 and 2020, the Manual Medicine department saw an above-average increase in consultation appointments and treatments compared with previous years. In response to this, a new consultant position was created in July 2020, which is currently filled by Dr. med. Anders Vetsch.
Expansion of the range of treatments: thermal ablation of nerve branches
In 2020, the Manual Medicine and Neurology departments laid the foundation for increased interdisciplinary cooperation and will be collaborating to offer a new therapy from the beginning of 2021: thermal ablation of nerve branches. The aim of thermal ablation is to switch off the transmission of pain signals in selected nerves.
In the thermal ablation of nerve branches, the needle is place at the target nerve before the tip of the needle is heated by a high-frequency current (to 60 to 90 degrees Celsius, depending on the technique). The heat changes the target nerve on a structural level (via Wallerian degeneration). This means that the nerve loses the ability to transmit pain stimuli, at least temporarily. As a rule, the therapy is effective for at least one year and can also be repeated afterwards without any problems. Thermal ablation is generally suitable for chronic pain conditions where the actual cause of the pain cannot be eliminated. Painful joints in the spine (facet joints, Figure Left) are probably the most common indication for thermal ablation. Another good indication is chronic pain originating from the sacroiliac joint, knee joint or nerves (Figure Right). Although thermal ablation is often indicated for chronic pain, it is only used as a complementary treatment in addition to the previous ultrasound- and image intensifier-guided infiltrations. In addition to manual therapy and trigger point treatments, joint infiltrations, neural therapy and infiltrations of the autonomic nervous system remain important interventions in the treatment of chronic pain.

Interdisciplinary Symposium

One of the few events to take place in the pandemic year, the 4th Interdisciplinary Symposium was held at Schulthess Klinik in January. Around 200 GPs/paediatricians and chiropractors attended the symposium’s presentations and workshops on our complete range of medical services, whereby plenty of practical advice was offered as well. From shoulders to feet, paediatric orthopaedics issues to prostheses, and sports medicine to cognitive screening – a wide variety of topics were covered, with tremendous interest among all participants. Dr. med. Gérard Hämmerle, Head of Manual Medicine, played a key role in designing the symposium structure and also presented two papers on the spine.
Further information
Internal Medicine

Our Internal Medicine department specialises in providing pre- and post-operative care to our patients as required. Incorporating such professional internal medical treatment into the clinic’s care programme enables even patients with complex underlying conditions to undergo orthopaedic surgery to improve their mobility and thus enhance their quality of life. During the coronavirus year, we suddenly found ourselves having to contend with a whole host of new tasks.
“Without our Internal Medicine team, we would never have made it through 2020 and the problems posed by the virus so well. Constantly resolute and reflective, the department has ensured that our patients and employees remain protected.”
Andrea Rytz, Director, CEO
In the spring, Internal Medicine was called upon within a short time to answer medical questions about the pandemic. It provided significant and ongoing support to the Directorate’s pandemic team. Within a very short time, an interdisciplinary protection concept had to be drawn up, implemented throughout the clinic and adapted to new situations as required. The protection of patients and colleagues has always been of paramount importance.
Questions about what to do if you experience symptoms, contact with Covid patients, testing options for staff, rules for patients and visitors and quarantine guidelines are only a fraction of the questions that the internal medicine team had to deal with on an ongoing basis in 2020. The initial situation had to be monitored constantly, and appropriate measures implemented with care and confidence. Thanks to this commitment, our employees and patients were always able to feel safe and the clinic operations were able to continue – as far as the measures allowed.
Further information
Medico-Legal Affairs

Last year, Schulthess Klinik once again offered a pooled expertise service for complex medical cases. Accident and court reports make up the bulk of the service, with liability reports also increasing in number over the last year.
“I was pleasantly surprised at how well meetings and conferences can function online.”
Dr. med. Georg Egli, Senior Consultant in Neurology and Head of Medico-Legal Affairs
The reports usually cover the specialties of orthopaedics, neurology, rheumatology and rehabilitation as well as psychiatry. We were able to see most of the patients concerned in person, even during the demanding Covid year, bar a few weeks in spring. However, professional exchange and further training have largely shifted to digital channels.
Pooled expertise in everyday clinical practice
The complex reports, for which preliminary expert assessments are often already available, tend to require a verified specialisation (for example, for a specific joint) as well as close interdisciplinary cooperation. Both elements are part of everyday life for the specialists at Schulthess Klinik, who are involved in these reports where their area of expertise is concerned. As these specialists all work actively in everyday clinical practice, they have a great deal of practical experience and are up to date with the very latest medical developments.
In the Medico-Legal Affairs department, this extensive expertise is pooled and then prepared for clients, taking into account the special medical insurance aspects.
Further information
Sports Medicine

The sports physicians at our Swiss Olympic Medical Center treat patients and athletes at every sporting level. They look after professionals, amateurs and young talent at our Swiss Olympic Medical Center at Schulthess Klinik or directly on the sidelines at games and events. 2020 was an exceptional year in which the team unexpectedly contributed a lot to sport as a whole, despite there being fewer sports accidents.
“2020 will be remembered as an instructive and humbling year of medicine in which, despite there being fewer sports accident consultations, we were able to contribute much more to sport than expected.”
Dr. med. Gery Büsser, Head of Sports Medicine and Head of the Swiss Olympic Medical Center
Social distancing and providing treatment from afar
Social distancing has been a cornerstone of combatting the pandemic since the beginning. Logically, joint sports were completely cancelled for a long time, and many of us took to exercising alone instead, including at home in front of the computer or smartphone, if only to keep moving a little. This had the positive effect of there being significantly fewer sports injuries. And it gave athletes and coaches time to focus more on targeting weaknesses and to explore a variety of other sports activities.
While emergency cases were allowed to continue to come to the clinic, we facilitated consultations and treatment remotely for other patients, in particular via video consultations. At first, being able to easily access a doctor from the comfort of your sofa seemed very convenient. Soon, however, the lack of tactile momentum and being able to feel muscle tone, record movement sequences and examine patients manually proved vital in making a good diagnosis. Nevertheless, the experience turned out to be extremely valuable, since assessing the situation by having patients describe their condition also demanded a greater degree of self-assessment and evaluation from athletes.
Intensive cooperation on protection concepts
The pandemic has also challenged the Sports Medicine team in an area we were not so conscious of before. For once, the focus was not only on the athlete with their complaints and inability to do sport, but on the shutdown of sports itself. While many things were no longer possible in amateur and popular sports, ingenious, clear-cut protection concepts had to be developed and rigorously maintained for top-level and professional sports. This was the only way, alongside the close cooperation with the cantonal and national authorities, to facilitate reasonably competitive sport in the professional sector at all. We were heavily involved in developing these kinds of protection concepts. Our knowledge and experience of the conventions and procedures in the various sports proved to be fundamental for us to able to effectively develop any protection concepts at all, and in such a way that they can be feasibly implemented.
The pandemic required and encouraged teamwork in an extreme way, not to mention responsibility for yourself and others. This was another positive development, as it put more focus on the essentials – in sports medicine, a branch of medicine that otherwise tends more and more towards a biomolecular physiology approach.
Social distancing in contact sports – from ice hockey to ballet – seems contradictory. However, in joint projects with a research group from ETH and agile partners from the plastics and sports industries, we were able to work together to develop methods to enable championships to be held in these sports as well, and with little risk. The year was characterised by protection concepts and measures which had to be adapted several times over, developments in combatting the spread of infection and interdisciplinary boards tasked with keeping sports feasible and safe, all of which required a high degree of solidarity and remarkable motivation from all involved.

Right: PET boxes around the players’ bench
Covid tests and support in returning to sport
For months, emergency Covid tests in teams and associations also shaped the way consultations or club visits unfolded. In 2020, we performed a total of 1,127 PCR tests and 742 rapid antigen tests. Much depended on the results and the consequent quarantine measures. The solid, straightforward contact with the authorities meant everyone was always able to find good solutions quickly.
Athletes suffering from coronavirus had to be supported in safely returning to sport. We carried out various clarifications for Covid-19-specific complications, for example. The exchange with specialists from the fields of cardiology and pneumonia involved in this proved to be very friendly, uncomplicated and goal-oriented, even under pandemic conditions.
In conclusion, 2020 can be summed up as an instructive and humbling year of medicine. Despite there being less frequent consultations about sports accidents, we were able to contribute much more to sport than we had expected. Both we and our athletes were able to get to know and appreciate each other from a new angle.
Further information
Therapy and Training

Our Therapy and Training department looks after patients, competitive athletes and amateur sports enthusiasts. This includes treatment for accidents or diseases of the musculoskeletal system, rehabilitation after surgery and a sports assessment for all performance levels, prevention and training support.
“Our employees were extremely flexible throughout the year. During the lockdown, for example, the sports therapy staff quickly set up a nursery service.
Markus Dohm-Acker, Head of Training & Sports Therapy
The Therapy and Training department team is made up of various specialists. Our physiotherapy service is divided into different areas: knee, hip, spine, shoulder and elbow as well as sports physiotherapy. This division and the close cooperation with the doctors at the clinic allow us to offer individual and efficient physiotherapeutic treatment. Ergotherapists support our patients in re-learning how to carry out everyday activities. Sports therapists and sports scientists get clients and patients moving healthily at Schulthess Training or as part of medical training therapy. Our performance diagnosticians provide a professional sports assessment.
A year that required flexibility
2020 was a year in which it was difficult to plan and which required us to be continuously on the lookout for new solutions. A flexible and imaginative team of colleagues is worth its weight in gold. During the lockdown in spring, we were hardly able to see any patients, and as most sporting events were cancelled, many external care days for our sports physiotherapists were also scrapped. Instead, our team helped out wherever they were needed, for example in the Patient Administration or IT departments. One highlight was the nursery service, which was set up from scratch for clinic employees to use for their children. The Sports Therapy staff set up the service and ran it with the support of Performance Diagnostics during the lockdown until 8 May. With so many sporty people taking care of them, you could be sure that the children had had enough exercise at the end of the day.

Patient care also increasingly needed new approaches. We sent out more than 1,200 home exercise programmes to our patients, provided support to many of them using Physitrack digital physiotherapy coaching or, if necessary, by telephone. We continuously adapted our security concepts to the new situation, much of which was all done while we worked from our home offices.
When it came to training, the focus was primarily on the health and safety of our clients and employees. We were thus constantly challenged with creating, adapting and implementing protection concepts so we could adapt our organisation to the constantly changing conditions and requirements. When the Schulthess Training subscription area had to remain closed, we also looked for and found alternatives to continue serving our clients, such as with videos, online courses or close support with training at home.
We also used the time to push ahead with projects launched last year, as well as to launch new ones. Among other things, this included the expansion of Rapid Recovery, a treatment concept for patients who have received an artificial hip or knee joint. The approach is designed to get patients back into normal, everyday life and activities soon after an operation. The most important point in physiotherapy is that patients are moving around on the day of their operation. We also laid the foundation for a particular group of our spinal column patients to allow us to build up this treatment concept in 2021.
New group training room
As of 29 June, the former therapy pool came into its own as a new large group training room, where not only training courses, but also new physiotherapy group courses such as GLA:D® have plenty of space to take place. We were also able to offer many former Aquafit clients suitable alternative training options.
Performance Diagnostics
Despite the pandemic, we conducted almost the same number of performance tests in 2020 as in the previous year. Most of these were with our professional athletes, but many were also with our loyal amateur sport clients. The most frequently performed tests were the lactate level test on the treadmill with training advice, the trunk strength test using a computerised testing device and the measurement of body composition.
Running Sport Forum

January saw our Running Sport Forum take place for the fourth time. A total of 250 running enthusiasts received input on all aspects of running, training and performance diagnostics. The speakers included Viktor Röthlin, Switzerland’s most successful marathon runner, Lukie Wyniger, producer of the reggae special on Radio SRF3, himself a keen marathon runner, and Tim Bartenstein, sports scientist and performance diagnostician at the Swiss Olympic Medical Center at Schulthess Klinik.
Ergotherapie
In 2020, the Ergotherapy team provided 19,239 treatments. While we were able to maintain patient care mostly in person at the clinic, except in spring, meetings and further training were largely moved to an online format. Five Ergotherapy staff members attended the first virtual congress of the European Federation of Societies for Hand Therapy (EFSHT) at the beginning of September (originally planned as a live event to take place in Basel). Two colleagues organised a session entitled “Neuropathic pain: Treatment options” with speakers from Canada, France and Switzerland.
Further information
Teaching, Research and Development

The Teaching, Research and Development department continuously contributes to the improvement of patient treatments with its scientific work. The department’s research teams work very closely with physicians at the clinic, which means scientific research can be incorporated directly into everyday clinical practice and, in turn, practical experience can influence research results. We also share our knowledge with colleagues in Switzerland and abroad through our publications, teaching activities and partnerships. In 2020, during the pandemic, much of this has been moved to digital channels.

“The support from our ICT department when we moved to a home office overnight was fantastic. Within a really short time, the infrastructure, including lots of special research programs, was up and running. THANK YOU!”
Teaching, Research and Development department
Research to continuously improve patient treatments
Quality also means knowing how patients are doing. This is why, at Schulthess Klinik, we keep in close contact with our patients, even after their treatment. Because we want to know how they are doing. In our long-standing tradition of research, we have conducted over 153,000 patient surveys since 2004. This way, we can make treatments better and safer.
Scientific output
Our researchers and doctors work in close collaboration and have once again produced numerous high-level scientific papers.
| 123 Original papers in peer-reviewed journals | 40 Peer-reviewed congress abstracts |
| 45 Reviews and other articles | 154 Lectures and training courses |
| 1 Book | 6 Dissertations and theses |
| 29 Book contributions | 11 Other |
During 2020, we completed 35 research projects with one or more publications, with another 115 ongoing projects at the end of the year.
Scientific awards in 2020
The study “Clinical thresholds of symptoms for deciding on surgery for trapeziometacarpal osteoarthritis” by our Hand Surgery department received the JHSE Editors’ Award. The award is given by the Journal of Hand Surgery – European Volume, the most renowned international journal in the field of hand surgery. The Editors’ Award is given to the best six articles in the journal in the previous year.
While many international congresses were cancelled in 2020 due to the pandemic, the EUROSPINE congress was still held, but this time in a new, virtual format. Two presentations from our Spine team were selected for the “Best of Show Session” , in which only eight of the almost 1,000 abstracts submitted were presented with the highest scores by the reviewers and the programme committee.
At the virtual DVSE congress (German Society of Shoulder and Elbow Surgery), two shoulder surgery publications were shortlisted to be nominated for the “Best Paper Prize”. Unfortunately, our team was not quite able to defend the title from 2019 – but to have two publications in the final selection was still a great success.
Professorship for Dezsö J. Jeszenszky

On 8 September 2020, the University of Debrecen in Hungary awarded Dezsö J. Jeszenszky the title of professor during a formal ceremony. The celebratory inaugural lecture took place at the Medical University of Debrecen in Hungary. His postdoctoral thesis entitled “New surgical procedures in the treatment of paediatric spinal column diseases” summarises what Prof. Dr. med. Dezsö J. Jeszenszky has achieved over all the years of his career for the treatment of children with scoliosis and other spinal disorders.
New collaboration with the European Spine Study Group and ETH Zurich
As an important member of the European Spine Study Group (ESSG), the Spine team of Schulthess Klinik has initiated a new collaboration between the ESSG and the biomechanics research group of Prof. Dr.Stephen Ferguson at ETH Zurich. The research project focuses on developing and using a musculoskeletal model. Its aim is to examine the influence of the spinal profile on the mechanical forces that occur in the adjacent vertebrae above a fused section of the spine. The study will help surgeons find the best spinal alignment for reducing potential secondary effects and associated mechanical complications affecting neighbouring vertebrae.
Preparation for the Swiss National Joint Registry, Hip and Knee (SIRIS)
In 2020, we completed our preparatory work for the Swiss National Joint Registry, Spine (SIRIS Spine). The aim of this national implant registry is to increase patient safety. Since 2004, Schulthess Klinik has been routinely documenting all operations in a format that is compatible with SIRIS (Spine Tango). Thanks to our preliminary work on the implementation of an electronic documentation system, we were able to meet the requirements of SIRIS without any problems and are ready to begin entering data in 2021.
Multicentre study on the arthroscopic treatment of rotator cuff tears
In June 2020, the first large prospective, multicentre Swiss cohort study documenting the outcome of patients undergoing arthroscopic treatment of a rotator cuff tear was launched, led by Schulthess Klinik and the University Hospital Basel. Since it started, more than 500 patients from 18 hospitals have been included in the study. The project is supported by the Swiss National Science Foundation (SNSF) and Swiss Orthopaedics and will run until 2024.
World’s first registry for acromioclavicular joint instability
The Shoulder and Elbow Surgery department has launched a new registry for patients with acromioclavicular (AC) joint instability. This register is the first in the world to focus so comprehensively on AC joint instability. The patients concerned are examined and interviewed at regular intervals for quality control purposes, which allows conclusions to be drawn about the functional outcome and patient safety.
Scientific projects in the Human Performance Lab (HPL)
In the Human Performance Lab, the focus of research projects is mainly to assess the function of the musculature and the joints or implants. The questions posed by the research projects are answered with objective measurements such as measurements of force or complex movement analyses. A number of promising projects have been initiated or completed, for example asking questions like “How can movement analysis be used as an additional tool for clinical routine?” or “Which molecular mechanisms lead to fatty degeneration of the hip musculature in patients with osteoarthritis in the hip?” or “What influence does hip shape have on the development of osteoarthritis in the hip? These projects are often carried out in collaboration with partners such as ETH Zurich, Balgrist University Hospital and Erasmus University Medical Center Rotterdam.
Knowledge gained through our research
The following are some highlights from our numerous publications with findings from our research that could have an impact on future treatment:
“What level of symptoms are patients with degenerative (caused by wear) curvature of the spine prepared to live with? This is a question that is also important for treatment and/or determining the effectiveness of treatment. From the survey of over 1,000 patients, we identified a level, which helps define a good treatment outcome for future studies.”
Mannion, A. F., Loibl, M., Bago, J., Vila-Casademunt, A., Richner-Wunderlin, S., Fekete, T.F., Haschtmann, D., Jeszenszky, D., Pellisé, F., Alanay, A., Obeid, I., Pérez-Grueso, F. S., Kleinstück, F. S., and the European Spine Study Group (2020). What level of symptoms are patients with adult spinal deformity prepared to live with? A cross-sectional analysis of the 12-month follow-up data from 1,043 patients. European Spine Journal 29(6): 1340-1352.
“Narrowing of the spinal canal in the lumbar region is a common degenerative disease of the spine. It is often unclear whether the patient would benefit most from surgical or conservative treatment. We therefore observed the outcomes of patients with this disease in a large multicentre study (with the University of Zurich and University Hospital Zurich, among others) for ten years. Schulthess Klinik provided by far the most patients for this study. Both groups of patients complained of very similar symptoms before the therapy, with the difference being that those patients who were subsequently treated surgically suffered from more severe pain in the buttocks and their symptoms had also worsened in the three months before the start of the study. Twelve months after treatment, the patients who had undergone surgical treatment had a better outcome than those treated conservatively, and tended to maintain that improvement over time.”
Burgstaller, J. M., Steurer, J., Gravestock, I., Brunner, F., Fekete, T. F., Pichierri, G., Ulrich, N. H. , Winklhofer, S., Porchet, F., Farshad, M., and LSOS Study Group (2020). Long-term results after surgical or nonsurgical treatment in patients with degenerative lumbar spinal stenosis: A prospective multicentre study. Spine 45(15): 1030-1038.
“Does hip impingement always require surgery? Often, specific types of physiotherapy can also significantly reduce the symptoms of patients with hip impingement. Our study therefore analysed which patients could benefit most from surgery or a specific form of physiotherapy.”
Casartelli, N. C., Valenzuela, P. L., Maffiuletti, N. A. and Leunig, M. (2020). The effectiveness of hip arthroscopy for the treatment of femoroacetabular impingement syndrome: a meta-analysis of randomized controlled trials. Arthritis Care and Research (Hoboken). doi: 10.1002/acr.24234. Epub ahead of print.
“Does the design of a joint prosthesis influence its movement? Using the unique moving fluoroscope measuring technique, we measured the movement of the knee prosthesis while walking and climbing stairs. The comparison of two knee prosthesis designs showed that even small changes in the geometry of the knee prosthesis can lead to a change in its movement.”
List, R., Schütz, P., Angst, M., Ellenberger, L., Dätwyler, K., Ferguson, S. J. (2020). Videofluoroscopic evaluation of the influence of a gradually reducing femoral radius on joint kinematics during daily activities in total knee arthroplasty. The Journal of Arthroplasty, 35(10): 3010-3030.
“Schulthess Klinik has been keeping a shoulder endoprosthesis register for more than 14 years. We have described the methods and properties of this register in a manuscript. This unique form of documentation was established in 2006 and since then, has provided valuable data for quality control and clinical research focusing on safety, function, quality of life and patient satisfaction after implantation of an artificial shoulder joint.”
Marzel, A., Schwyzer, H.-K., Kolling, C., Moro, F., Flury, M., Glanzmann, M. C, Jung, C., Wirth, B., Weber, B., Simmen, B., Scheibel, M. and Audigé, L. (2020). The Schulthess local Shoulder Arthroplasty Registry (SAR): cohort profile. BMJ Open ,10(11): e040591.
“Even after five years, patients with the CapFlex prosthesis on the proximal interphalangeal joint are doing well. Our patients showed a significant improvement in pain and hand function compared to before surgery and good finger mobility. There were only a few complications, which were comparable or even milder than with other types of prostheses for the proximal interphalangeal joint.”
Reischenböck, V., Marks, M., Herren, D. B. and Schindele, S. (2020). Surface replacing arthroplasty of the proximal interphalangeal joint using the CapFlex-PIP implant: a prospective study with 5-year outcomes. Journal of Hand Surgery (European Volume). doi: 10.1177/1753193420977244. Epub ahead of print.
“From a health perspective, reconstruction of a torn rotator cuff (shoulder tendon) can help many patients. But does the intervention also make economic sense? The study compared shoulder function, quality of life and costs before and after surgery in 153 patients. The costs include both the direct medical costs and the loss of productivity at work. The cost-utility analysis in the study shows that arthroscopic rotator cuff reconstruction is a cost-effective procedure that significantly improves patients’ quality of life and shoulder function.”
Grobet, C., L. Audige, K. Eichler, F. Meier, B. Brunner, S. Wieser and M. Flury (2020). Cost-utility analysis of arthroscopic rotator cuff repair: A prospective health economic study using real-world data. Arthroscopy Sports Medicine, and Rehabilitation 2(3): e193-e205.
“We know that ossification of soft tissues around a hip prosthesis can occasionally occur. But does this also have an effect on the outcome? Our study shows that smaller ossifications, which frequently occur, rarely have any relevance for the patient. However, the rare large ossifications have a negative effect on function and patient satisfaction.”
Rüdiger, H. A., Dittrich, M., Robinson, J., Mansour, T., Schwab, T., Stadelmann, V. A. and Leunig, M. (2020). The impact of heterotopic ossification on self-reported outcomes after total hip arthroplasty using the direct anterior approach. The Journal of Bone and Joint Surgery 102(Suppl 2): 91-98.
Research and teaching partnerships
2020 saw the launch or advancement of many exciting cooperation projects: For example, a project of the Swiss National Science Foundation (SNSF) and University Hospital Basel which seeks to evaluate the results after arthroscopic reconstruction of the rotator cuff. With Prof. Dr. Stephen Ferguson from ETH Zurich, a doctoral position has been created with the aim of making movement analysis accessible for routine clinical use.
In addition to the important cooperation partners ETH Zurich and University Hospital Basel, our scientific network includes numerous other national and international partners and interest groups, such as the Swiss Federal Institute of Technology in Lausanne (EPFL), Zurich University of Applied Sciences (ZHAW) Winterthur, the University Hospital Zurich, the Lausanne University Hospital (CHUV), Charité – Universitätsmedizin Berlin, Balgrist University Hospital, AO Foundation, Foundation for Patient Safety Switzerland, European Spine Study Group (ESSG), Univers Revers Study Group, Arthroscopic Rotator Cuff Repair outcome Prediction Group, University of Oxford, University of Utah, Humanitas University, Medical University of Vienna, University of Turin and University of Alcalá.
Further information
Inpatient Departments Nursing Services

Our nursing department cares for our patients in a personalised, professional, interdisciplinary and future-focused manner in accordance with our care mission statement. This is why 195 employees in 139 full-time positions, divided into five professional groups, were working in five inpatient departments in 2020. The team navigated the pandemic year 2020 masterfully and with a great deal of flexibility and team spirit.
“The excellent support in the team and the mutual exchange of information helped enormously to master working at this very particular time.”
Valbone Thaqi, registered nurse S6
Corona as task master
The coronavirus pandemic has placed numerous demands on Nursing Services on many levels. Thus, it was an ever-present topic and task in the everyday operation of the hospital. All employees from the different areas of the hospital were faced with dealing with the new situation. The nursing staff also had to redesign processes in order to be able to provide safety and comfort for our patients at the levels we usually strive for. We were always able to achieve this goal because our nursing team reacted to the situation with flexibility and openness and saw themselves as part of a team.
The excellent communication and constant contact within the team and between the departments dealt with uncertainties and fears well and promoted a sense of confidence. The staff actively dealt with the altered situation and provided support where necessary, including in other health institutions.
Bed occupancy increased despite shutdown
Due to the corona-related lockdown, the set targets for bed occupancy were actually way behind at the beginning of the year. However, thanks to excellently implemented bed management and the great team work shown by everyone involved, we were in fact able to record an increase in occupancy at the end of the year compared to the previous year’s figures.
Host care
The department heads now take care of feedback personally during our clients’ stay with us. This change has further strengthened the quality we offer and our focus on service, which is now even more noticeable to our clients as a result. In the role of host, they can respond even better and more quickly to client concerns and feedback. Consequently, the way we implement our care mission statement is continually improving and the client is even more at the centre of our actions.
Further information
Operations

More than 9,000 operations are performed every year in Schulthess Klinik’s operating theatres, which are fitted with state-of-the-art equipment. Standardised procedures that are continuously reviewed ensure maximum safety and quality for our patients. In addition to the doctors on the staff, the following professional groups also play an important role in this: anaesthesiologists, surgical nursing/surgical technology, positioning specialists, operating theatre logistics, nurses, healthcare assistants, cleaning staff and nursing assistants.
“The spontaneous offer of Schulthess Klinik staff to support us in treating patients suffering from Covid-19 in the intensive care and monitoring ward, as well as their extremely efficient implementation, were, for me, one of the most positive experiences of cooperation in practice in my entire medical career and were also greatly appreciated by my colleagues and by Klinik Hirslanden.”
Prof. Dr. med. Reto Stocker, Head of the Institute for Anaesthesiology and Intensive Care Medicine at Klinik Hirslanden, Zurich
Sticking together through the crisis
So we could all cope with the Corona pandemic, the Zurich hospitals worked closely together. Klinik Hirslanden and Schulthess Klinik were close cooperation partners. For example, Schulthess Klinik loaned specialist staff from Anaesthesiology and IMC (intermediate care) to Klinik Hirslanden for several weeks. The collaboration was a roaring success. Our specialists were trained in handling Covid patients and the procedures in place on the Hirslanden intensive care unit. At the same time, they were able to relieve pressure on the Hirslanden team by helping out in the intensive care unit. This cooperation under stressful circumstances has brought us much closer together. As a thank you, our team was invited to the summer party at Klinik Hirslanden, which took place in the open air in accordance with coronavirus and social distancing rules.
Time used for standardisation and process optimisation
When part of the operating theatre team helped out at Klinik Hirslanden during the lockdown in the spring, the rest of the team at Schulthess Klinik was certainly not idly standing around. One of the ways we used our time was to further optimise and expand our operating theatre management. For example, we implemented a number of standard operating procedures (SOPs) and set up an operating theatre management key performance indicator (KPI) system. The standardisation of the incision time for all surgical areas is another example of one of many standardised procedures that ultimately contribute to the continuous improvement of patient safety, efficiency and quality. We also passed the audit for ISO recertification with flying colours.

Right: department-specific storage of the instrument containers in the paternoster (Rotomat)
Every cog counts
Our operating theatres are home to a team consisting of a wide range of professional groups, nationalities and cultures, working hand in hand for our patients. Not only in an individual area, but also across different areas and specialisations, every collective thought and coordinated action is important – basically: every cog counts. This makes the transparent communication and cohesion that plays out every day all the more important. The surgical lounge is an important hub. This is where people eat together, drink coffee (39,900 cups in 2020!) and exchange ideas – all as a cohesive team unit that we were able to safeguard and keep together in 2020, thanks to our effective protection concept.
Further information
Radiology

The Radiology department at Schulthess Klinik is equipped with state-of-the-art, dose-reduced X-ray equipment. A particular specialisation is the production of complete digital leg and spine images (EOS) in 2D (animated film) and 3D technology.
“2020 has made our team even stronger. We were all incredibly willing and prepared to protect each other. And our flexibility in adapting to new and changing processes that were dictated by the coronavirus was just as impressive.”
Danijela Zivkovic Jurisic, Department Manager Radiology
Our Radiology department also works closely with the Medical Radiology Institute (MRI), which is housed on the premises of Schulthess Klinik. This gives our patients direct and uncomplicated access to precise cross-sectional imaging examinations directly at the hospital.
Expansion of our radiology activities
Since the end of September 2020, our Radiology department has had an additional X-ray room. This, together with more staff, creates more capacity for the 250 to 300 patients we treat on a daily basis and shortens waiting times. The new digital ticketing system efficiently and discreetly guides patients to their examination. This expansion in terms of space and administrative capacities follows the steps to improve the radiological equipment, which were already underway in 2019.
In 2020, the Schulthess Klinik Radiology department became the first radiology department in Switzerland to put the new Precision i5 X-ray machine into operation.
Precision i5 is a high-quality digital X-ray system that offers high image quality, clinical flexibility and superior workflow for a wide range of X-ray applications. With the motorised, tilting wall bucky, special exposure capacities, for example for the ankle and shoulder, can be adjusted more quickly and easily than the previous set-up. In addition, the motorised pendulum movement enables better tube tilting adjustment to the patient’s anatomy, which is very important for demanding orthopaedics. The Precision i5 X-ray unit thus offers high-quality imaging, and does so with a low radiation dose for maximum patient safety.