Medical condition Hip prosthesis – the artificial hip joint
Hip replacement is one of the most successful operations to treat painful hip osteoarthritis. Initially, osteoarthritis can be treated conservatively, i.e. without surgery. The use of an artificial hip joint is considered depending on the level of suffering (intensity of pain) and limitation of mobility, as well as the patient’s quality of life. Now considered a routine operation, this mostly painless procedure can restore the original mechanism of the hip joint, meaning that, for the patient, the artificial joint feels similar to a natural one.
Find out more about the use of hip prostheses below. The explanations summarise the current standard of knowledge. They are primarily based on scientific work carried out by Schulthess Klinik staff over the past 20 years.
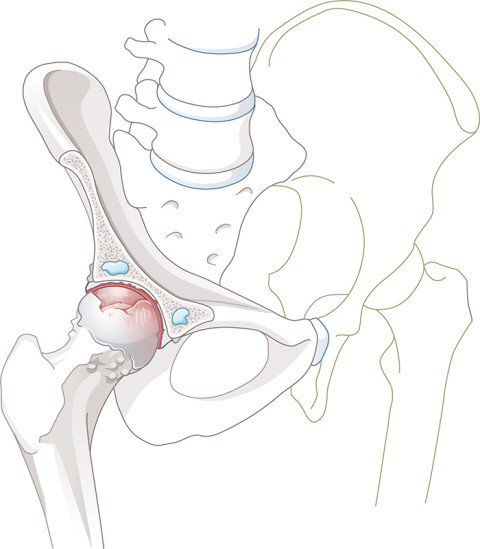
Anatomy of the hip joint
The hip joint is made up of the hip socket and the femoral head. These are covered by a smooth layer of cartilage, and the synovial fluid between these two surfaces absorbs friction and further lubricates the joint. The rim of the hip socket is surrounded by the labrum, a ring of fibrous cartilage, which seals the joint. Finally, the entire hip joint is surrounded by a tight capsule and a powerful layer of muscle.
When it comes to locomotion, the gluteal muscles (abductors) play a particularly key role, as they keep the pelvis horizontal when walking and thus prevent limping. Important nerves run along the front and back of the hip joint. The blood vessels, which supply the extremities, run into the leg beneath the groin along the front surface of the hip joint.
As a ball-and-socket joint, the hip joint enables movement in different directions. It also has to distribute the weight of the body to the legs and ensure the stability of the upper body.
Hip osteoarthritis
The most common condition affecting the hip joint is osteoarthritis, when the layer of cartilage protecting the femoral head and the hip socket is worn away. The joint loses its fit, the bone forms bony deposits (osteophytes) around the edges, and wear particles develop, which cause inflammation and pain. The onset of hip osteoarthritis can be as early as between the ages of 30 and 40, but is usually seen between the ages of 50 and 60.
The causes of hip osteoarthritis can vary widely. While it was previously believed that osteoarthritis was wear of the joint cartilage purely as a function of age, it is now known that an awkward shape of the femoral head and hip socket, heavy strain, accidents and other illnesses increase the risk of osteoarthritis. You can also learn more about causes and symptoms on the hip osteoarthritis page (available in German only).
Surgical treatment
When suffering is severe and quality of life badly impaired, use of an artificial hip joint (prosthesis) must be considered. It is always the patient who decides what constitutes suffering and the severity of this.
Total hip replacement is one of the most successful operations in orthopaedics. The unhealthy femoral head and part of the femoral neck are removed. The natural hip socket is then smoothed and the artificial socket anchored fixed into the pelvis. A canal running down into the femur is then prepared, into which the stem is inserted. The head of the prosthesis is finally attached to the stem and the two parts of the artificial hip joint are joined together. In order to achieve a stable prosthesis with the correct leg length and muscle tension, attention must be paid to the correct size and position of the prosthetic components. This is determined for each patient based on their pre-operative X-ray image so that patient-specific plans can be made for the operation.
At Schulthess Klinik, an anterior, minimally invasive approach is almost exclusively used to insert the prosthesis. This approach is considered to be the gentlest way of exposing the hip joint, especially as it runs down through a natural layer between the muscles and thus does not result in any significant muscle damage. Alternatively, a lateral or posterior approach to the hip joint can also be taken, but this involves the partial detachment and reattachment of muscles.
The main focus of today’s minimally invasive surgical techniques is to avoid soft-tissue damage. In most cases, just a short skin incision (<10 cm) is sufficient. A few years ago, we also introduced a transverse skin incision for the anterior approach, known as a bikini incision, instead of the traditional longitudinal incision. This follows the skin creases and results in more cosmetically attractive scars that are easier to hide under underwear – hence the name.
Hip operations are either carried out under general anaesthetic or with a spinal anaesthetic. The operation takes about one hour. Generally, the affected hip can bear full weight again immediately after surgery.
Hip prosthesis materials
Hip prosthesis materials
Hip prosthesis stems are made from various metal alloys (titanium, cobalt-chromium). The head of the prosthesis itself is made from ceramic or metal and is placed onto the cone of the stem. Different implant sizes and geometrics enable an exact reconstruction of the individual anatomy. The socket is also made from a metal alloy (in most cases titanium) and is fitted with a ceramic or plastic insert (polyethylene). These materials are perfectly compatible with the body – allergies to titanium, ceramic or polyethylene are largely unknown.
Nowadays, cement-free implants made from titanium alloys are preferable when the bone quality is good. These fix securely into the bone (primary stability). Within 4-8 weeks the bone then grows onto the porous titanium surface, helping to fix the implant in place (secondary stability). When the bone is brittle (e.g. osteoporosis), a cemented prosthesis is used instead. Depending on the type of prosthesis used, it may provide medial support (collar) or may also be used without a collar.
At Schulthess Klinik, we only use prostheses that have proven themselves on the market and are ranked highest in the relevant registries. Schulthess Klinik does not use custom-made prostheses.


Follow-up treatment and rehabilitation
The first steps are taken on the day of the operation itself, using two walking sticks and under the guidance of a physiotherapist. After two to four days, the patient can leave the clinic. We expect the trend towards shorter bed rest periods to continue.
With the minimally invasive surgical techniques used today, walking sticks are only needed for two to four weeks. Depending on the surgical technique used, however, certain precautions and lifestyle rules should be followed in the first few weeks with regard to certain movements and loads.
In most cases, we use absorbable sutures that do not need to be removed. When the first check-up has been carried out by the surgeon (usually after six weeks), joint mobility and load can be progressively increased.
The period of inability to work ranges from three to twelve weeks depending on the physical demands of the patient’s work.
After the inpatient stay, outpatient physiotherapy is recommended. The aim of this treatment is to enable hip joint function to be restored quickly. This initially improves mobility and coordination, and then builds strength. The intensity of the exercises is continuously adjusted to the patient’s load-bearing capacity and individual goals.
The resumption of sporting activities should be discussed with the doctor and physiotherapist. Driving is usually possible again after four to six weeks if walking sticks are no longer needed.
No dental work after a hip operation
Any foreseeable dental work should be carried out before a hip operation. Good and regular dental hygiene is important. Dental work should not be carried out in the first three months after the hip operation unless due to an infection. Before dental procedures, it is important to rinse the mouth with an antiseptic. Prophylaxis with antibiotics before going to the dentist is only considered in rare cases in immunosuppressed patients. (Recommendation in accordance with the review article of the expert group 'Infection' of Swiss Orthopaedics, Sendi et al, J. Bone Joint Infect 2016; 1: 42)
Lifespan of a hip prosthesis and prosthesis replacement
The lifespan of a hip prosthesis is estimated to be at least 15 to 25 years, based on the materials currently used. With advancing technology and new materials, we can expect an even longer lifespan in the future.
Lifespan also depends heavily, however, on the amount of strain and on other factors such as bone quality, etc. Stop-and-go sports can have a negative impact on the prosthesis and should be avoided.
Reasons for changing the prosthesis
Even an artificial joint produces friction and will wear over time, potentially causing inflammation. The bone then recedes from the prosthesis and the prosthesis becomes loose, affecting either the socket, the stem or both. The most common reasons for changing a hip prosthesis (revision) are wear and loosening, repeated dislocation (luxation), bone fractures and infections.