News Research award: Successful therapy for painful lateral disc herniation from a patient’s perspective
A Schulthess Klinik research group has received the «Outstanding Special Poster» award from the International Society for the Study of the Lumbar Spine for its research report on a therapy for painful lateral disc herniation.
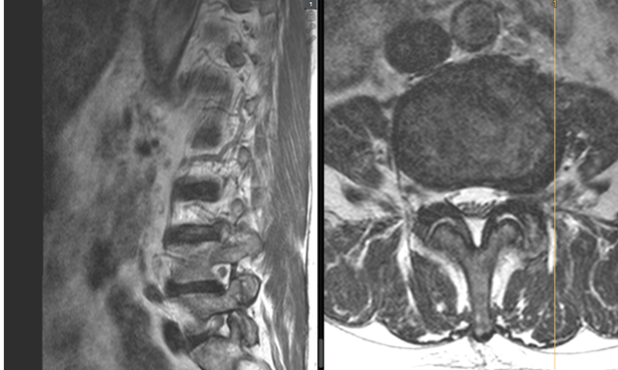
Cases of (extreme) lateral disc herniation that lead to compression of the exiting nerve root are not common and often very painful (Figure 1). Studies solely focused on such cases of disc herniation are rare and, as a result, mostly only present low case numbers. As a large Spine Centre, we have the opportunity to collate and analyse sufficient amounts of case data, even on this rare condition.
In most cases, lateral (paramedian) access is used in relation to operative microsurgical therapy for lateral disc herniation; this is referred to as the far-lateral approach (FLA) or the Wiltse approach. The most important study parameter was defined as the patient-based clinical outcome (PROM, patient-reported outcome measure) up to 2 years after surgery. This was used to work out which clinical and radiological factors are associated with each outcome.
Background
From an anatomical point of view, the different segments of the spine differ from one another. Specifically, the L5/S1 segment, the junction between the lumbar spine and the sacral bone, is unique and can pose a particular challenge. To complicate matters, accessibility for the surgeon at the L5/S1 level is impeded by the pelvis. Lateral disc herniation is often connected to degenerative changes to segments. Hence, scoliotic changes (lateral curvature of the spine), for example, may intensify the pressure on the nerves.
Up until now, any association between the affected spinal segment and lateral curvature (coronary asymmetry) on the one hand and patient-reported outcomes on the other, following microsurgical decompression for this kind of disc herniation, has not been studied.
Methodology
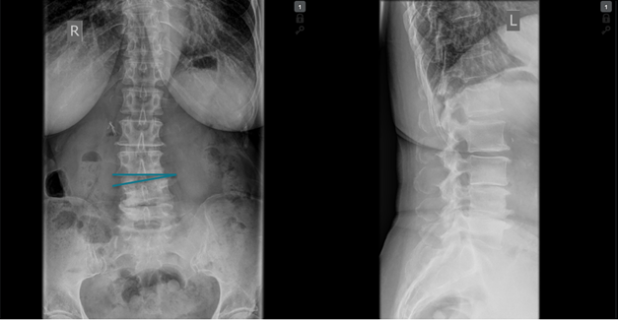
Patients who underwent microsurgical decompression using the FLA technique between 2005 and 2020 were selected to take part in the study. The coronal segmental Cobb angle (CSCA) was measured on the pre-operative, posteroanterior X-ray (Figure 2). The primary end point was the Core Outcome Measures Index (COMI) score at the two-year follow-up examination (2FU). This involved a patient questionnaire (PROM), which, alongside pain, included questions on function restrictions in day-to-life and at work, symptom-specific wellbeing and quality of life.
Results
The final study group comprised 148 patients, whilst the control group (standard disc herniations) included 463 patients. All patients across both the study and the control group demonstrated a significant decrease in the COMI score (i.e. an improvement in their symptoms) from the pre-operative phase to the two-year check-up (p < 0.0001). Results were better (COMI score lower by 0.6 points) for patients treated at the higher lumbar vertebrae segments than those treated at the lowest level, L5/S1 (p=0.03). As well as this, in the study group, there was a statistically significant correlation between the intervertebral angle (CSCA) measured pre-operatively and the change in the COMI score two years post-operation (p < 0.001).
The association could also be found in a multiple regression analysis, which was controlled for confounding factors. An increase in the CSCA by one angular degree was linked to a 0.3 point drop in the COMI score at the 2FU (p=0.008).
Conclusions
Surgical treatment for lateral disc herniation results in good outcomes overall as far as patient reporting is concerned. Outcomes are reduced at the anatomical level L5/S1 in general and within the study group showing more pronounced intervertebral angles (tilting of the segment). For such cases, alternative surgical techniques may be preferred.