Knee Surgery
Annual Report 2022

Our Knee Surgery department is the largest Swiss reference centre for knee joint replacement, including complex revision surgery. In addition to prosthetics, our specialists also offer the entire spectrum of joint-preserving surgical options. Axial corrections, fracture treatment and cartilage repairs are just as much a part of the department’s work as complex ligament reconstructions.
High case numbers as a foundation for high quality
Thanks to our high case numbers and the specialisation of our departments, each surgeon has a very high level of experience and practice. Last year alone, we inserted 771 total knee prostheses and 174 partial knee prostheses. We also performed 140 knee prosthesis revision procedures.
But it is not just the doctors who have extensive experience; the same can be said for other departments such as nursing, physiotherapy or operating theatre specialists. Thanks to the high number of cases, they have had valuable practice in dealing with the various conditions we treat.
As an innovative clinic, we are constantly moving forward and always make a point to keep up with the latest technologies and techniques. Last year, for example, 104 operations were performed with “ROSA”, an orthopaedic robot. We also evaluate how patients can benefit from new surgical techniques on an ongoing basis.
Revision rate: over three times better than the Swiss average
You become better at and more practised in the things you do often. This is also reflected in the data in the Swiss National Joint Registry SIRIS. The registry allows data on complication rates relating to individual hospitals and implants to be monitored and compared. For example, the latest publicly available report lists a two-year revision rate for knee prostheses of 1% for Schulthess Klinik, which is more than three times lower than the Swiss average (3.4%), despite Schulthess Klinik having the second highest number of cases in Switzerland. (SIRIS report 2022; report period 01.01.2016 to 31.12.2019.).
This means that, after a hip or knee replacement operation, significantly fewer Schulthess Klinik patients require revision surgery than the average in hospitals across Switzerland.
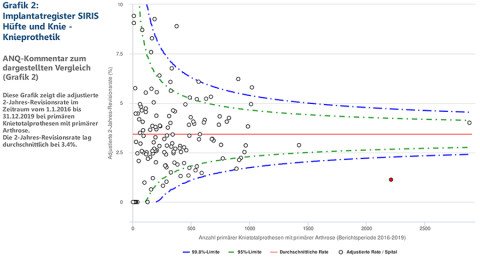
Image source: www.anq.ch
Low infection rate with primary knee replacements
Another important instrument for measuring quality is the Swiss Registry for Postoperative Infections Swissnoso. Since 2009, the majority of Swiss hospitals have opted to use it. To date, the most important quality criterion has been the rate of infection one year after surgery, which stands at 0% for the current evaluation period from 1 October 2020 to 30 September 2021 at Schulthess Klinik (Swiss average: 0.79%). Compared to the previous year (0.43%), the infection rate at Schulthess Klinik has dropped.
The data is now recorded 90 days after surgery. For the first evaluation period, from 1 October 2021 to 30 September 2022, the infection rate was 0.47%, which is roughly in line with the Swiss average (0.43%).
On the move with robot-assisted surgery

For almost two years now, the knee surgery team has been regularly using the orthopaedic robot “ROSA” in operations. The device supports the surgeon when inserting knee prostheses in areas such as guiding incisions and aligning the components. The entire team now has experience of around 250 operations.
The benefits are evaluated on an ongoing basis. We have already carried out a scientific evaluation and the first publications are expected in 2023. Dr. med. Gregor Baumann in particular is very pleased with the success of the technology. The operation time with ROSA has already been significantly reduced, with surgery only lasting about 10% longer than with the standard procedure. The precision of the surgical steps (incisions) is extraordinarily high. In addition, the “virtual component placement” performed during the surgery is a good teaching tool for beginners and more advanced orthopaedic surgeons alike.
We cannot yet prove whether this surgical technique also delivers a benefit for patients. However, the area of prosthetics is currently undergoing rapid change worldwide, with various principles being reviewed and altered. Here in particular, the orthopaedic robot can make an important contribution in further optimising the already good results.
Cruciate ligament strengthening
After reconstruction of the anterior cruciate ligament, patients may experience continued rotation instability. This can lead to a worse outcome for the patient or the replacement may even fail, which poses a challenge for the orthopaedic surgeon. Anatomical variations, additional injuries (especially involving the meniscus), revision surgery or pre-existing ligament laxity are possible reasons for the remaining instability.
In the last 10 years, a structure in the knee joint that had previously been somewhat forgotten has come back into focus for surgeons and scientists: the anterolateral ligament (ALL). Many studies show that this structure can have an effect on stabilising rotational movement. An injury to the anterior cruciate ligament is very often accompanied by a twisting of the knee joint, which may injure the ALL.
Until now, the practice has been to treat patients in which this occurs and also those with a renewed tear of the cruciate ligament with additional stabilisation at the front and side of the affected area. This can be done using various surgical techniques, which have shown comparably good results in studies. Recent and widely accepted data now shows that, in particular, young, athletically active patients without instability also benefit from this kind of additional anterolateral stabilisation. This procedure can reduce the risk of a new tear by up to four times.
That is why we are increasingly treating patients with this technique as part of a first operation and we discuss this treatment option with patients individually on a case-by-case basis. The results so far have been very promising: “The patients showed good stability and strength development subjectively and objectively in the follow-up checks, with no restriction of mobility or increase in pain,” explained Prof. Dr. med. Michael Worlicek, who treated many patients using this approach last year. “So the additional and necessary small incision is having a good outcome. Whether this also improves outcomes in the long term remains to be seen with future scientific results.”
This also applies to knee surgery. Relying on a strong foundation of experience and science, we are always moving forward for the benefit of the patient.



